Resources for each step of the treatment journey with AUSTEDO XR
Downloadable resources
Use this tool for the assessment and routine monitoring of patients at risk of TD.
A tool developed and published by a consensus panel of experts to help guide the routine monitoring and evaluation of TD impact.
Fill out this form to enroll your patient in Teva Shared Solutions® (for patients taking AUSTEDO XR).
Fill out this form to enroll your patient in Shared Solutions (for patients taking AUSTEDO BID).
Use this template to write an appeals letter, which payers may need to appeal a denial of coverage for AUSTEDO® XR (deutetrabenazine) extended-release tablets or AUSTEDO® (deutetrabenazine) tablets.
Use this template to write a letter to establish medical necessity, which payers may require for treatment with AUSTEDO XR or AUSTEDO.
This brochure provides an overview of support services offered through Shared Solutions, including working with pharmacies to fill prescriptions and managing prior authorization and appeals.
Downloadable resources for your patients with TD
A useful resource for patients as they begin their treatment journey. Patients and their carepartners can use this tracking tool to record when they take their treatment, as well as any changes in their TD.
This brochure provides answers to important questions your patients with TD and their carepartners may have when starting treatment.
This brochure provides an overview of patient support services offered through Shared Solutions, including help with access and affordability.
Videos to help you support your patients with TD
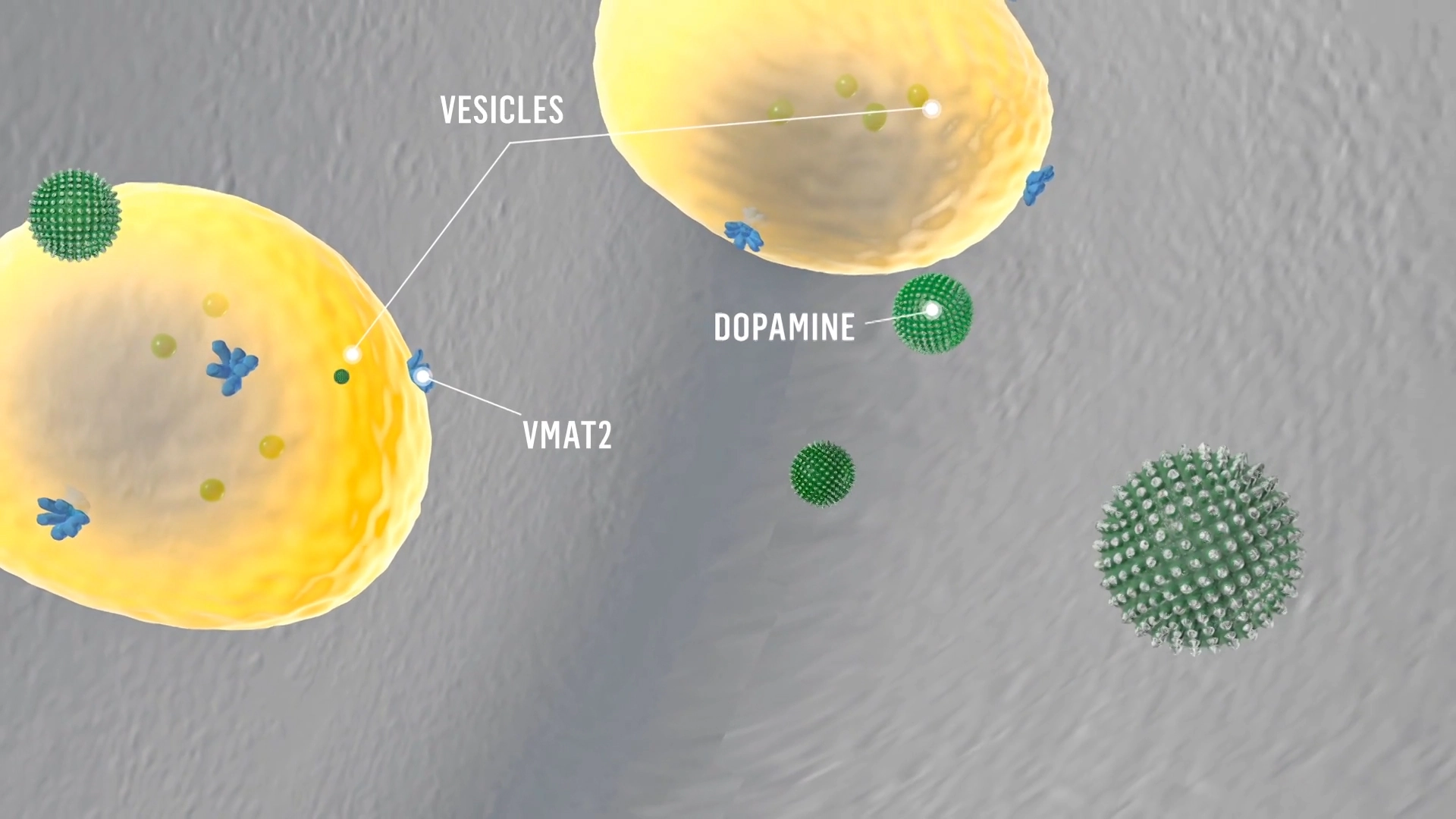
Mechanism of Action
VMAT2 inhibition can help regulate dopamine function.1
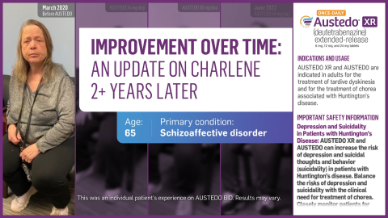
Improvement Over Time
See an update on Charlene and her treatment journey 2+ years later.

The Impact of TD: Charlene and Squirt
When Charlene’s TD was at its worst, the movements in her hands, legs, and feet got in the way of her caring for her best friend, Squirt. See why AUSTEDO was the right move for her.
Faces of TD: Patient case studies

Brian, a patient with bipolar disorder, who has had his routine disrupted by TD.
Patricia, a patient with major depressive disorder, who is also taking an antihypertensive.
TD Talks: Informative videos on TD evaluation and treatment
Amber Hoberg, PMHNP-BC, discusses the importance of assessing and managing TD.
Demystifying EPS: TD Is Distinct—a 3-part series on the importance of differential diagnosis
Chapter 1: Considering the landscape of antipsychotic usage.

Chapter 2: Opposing mechanisms of TD and drug-induced parkinsonism (DIP).
Chapter 3: Differential diagnosis of TD.
TD virtual assessments, demonstrated by Dr. Arvinder Walia

A long virtual assessment, with full view of the patient’s body.
A short virtual assessment, without full view of the patient’s body.
For more videos, visit the YouTube page.
EPS, extrapyramidal symptoms; VMAT2, vesicular monoamine transporter 2.
REFERENCE: 1. Solmi M, Pigato G, Kane JM, Correll CU. Treatment of tardive dyskinesia with VMAT-2 inhibitors: a systematic review and meta-analysis of randomized controlled trials. Drug Des Devel Ther. 2018;12:1215-1238.








